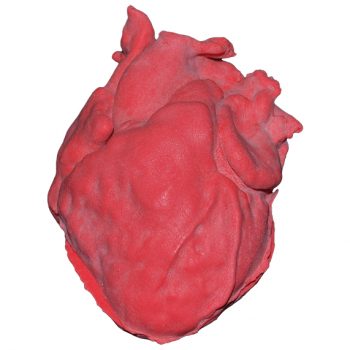
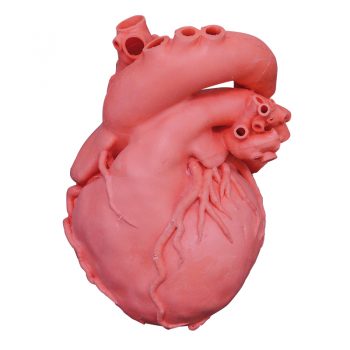
Product information “Syphilitic Aneurysm”
Clinical History
A 61-year old male presents with exertional anginal chest pain and dyspnoea. He has had these symptoms for 6 years with increasing severity. On examination, he is cyanotic and tachycardic with a collapsing pulse. A swelling was noted on the right side of his neck. There was a thrill in his carotid artery. The apex beat was displaced inferolaterally. A loud systolic and diastolic murmur was auscultated in the aortic area. Chest X-rays showed cardiomegaly with a large rounded lesion in the right upper mediastinum continuous with the heart shadow with radiographic evidence of cardiac failure. Blood tests were positive for anti-treponemal antibodies. The patient‘s condition deteriorated and he died of cardiac failure.
Pathology
This specimen is the patient‘s enlarged heart, including the aortic arch and descending aorta. The ascending aorta is dilated up to 7 cm in diameter, and is expanded superiorly by a large aneurysmal bulge 11 x 13 cm in diameter. This has been opened to display the wrinkled scarred intimal surface. There is also marked atheroma of the intima. The innominate, left common carotid and subclavian arteries have been displaced towards the patients left by the aneurysm. On the internal surface of the aneurysm there is a ridge-like thickening 5 mm high. This is the site of attachment of the pericardial sac externally. There is marked congestion of small blood vessels in the adventitia of the aorta. This is a syphilitic aneurysm of the arch of the aorta.
Further Information
Syphilis is a chronic infection caused by the spirochete Treponema pallidum. Sexually transmitted infection is most common but it may also be congenitally acquired by transplacental transmission of the bacteria. Those who have the higher risk of syphilis infection include those of a sexually active age, intravenous drug user, HIV-infected patients and male same sex relationships. Syphilis infection rates decreased significantly with the introduction of penicillin in 1943; it remains the main treatment today. However, the infection rate has been increasing since the early 2000s.
Syphilis is divided into three clinical stages with distinct clinical and pathological features with characteristic proliferative endarteritis affecting small vessels.
Primary syphilis occurs usually 3 weeks after initial infection. This manifests typically as a single, painless and erythematous lesion called a chancre at the site of inoculation. The syphilis spreads throughout the body from this chancre which then heals spontaneously after 3 to 6 weeks.
Secondary syphilis occurs weeks to a few months after the primary chancre resolves in 75% of untreated patients. During this stage patients commonly have generalised symptoms, such as malaise and lymphadenopathy and skin rashes. Palmar/plantar rashes are the most frequent site but rashes can be diffuse. These rashes can be maculopapular, scaly or putular.
Condylomata lata are elevated gray plaques that arise on the moist mucous membranes such as oral or genital regions. Other less common manifestations include hepatitis, gastrointestinal invasion or ulceration and neurosyphilis – discussed below.
Tertiary syphilis has three main characteristics: cardiovascular syphilis, neurosyphilis and gummatous syphilis. These occur after a latent period of 5 years or more in ? of untreated patients. Cardiovascular syphilis involves an aortitis for which the exact pathophysiology is unclear. The vasculitis involves the ascending thoracic aorta leading to progressive dilation of the aortic root. This can lead to aortic valve insufficiency from dilation of the aortic valve ring. Endarteritis of the vasa vasorum leads to scarring
of the media with loss of muscle and elastic tissue leading to the formation of aneurysms. Clinical manifestation usually happens 15-30 years post initial infection.
Neurosyphilis can be symptomatic or asymptomatic. It occurs in 10% of untreated patients. Early clinical manifestations include headaches, meningitis, hearing loss and ocular involvement, most commonly uveitis, causing vision loss. Late manifestations can occur up to 25 years post initial infection. Main features are meningovascular neurosyphilis, paretic neurosyphilis and tabes dorsalis. Meningovascular involvement involves chronic meningitis and endarteritis which can lead to strokes. Tabes dorsalis is caused from degeneration of the posterior columns within the spinal cord. This causes loss of proprioception, ataxia, loss of pain sensation, and loss of reflexes. Paretic neurosyphilis is caused by invasion and damage of the brain parenchyma, most commonly the frontal lobes. This leads to progressive cognitive impairment and mood disturbance.
Gummatous syphilis is characterised by the formation of nodular lesions most commonly bone, skin and mucosa of the upper airway and mouth called gummas. These can occur anywhere including viscera. The formation of gummas is rare but occurs more frequently in HIV-infected patients. Skeletal involvement causes pain and pathological fractures.