A 56-year-old woman with 6 months of intermittent headache and vomiting was admitted to hospital comatose after a grand mal seizure, and failed to regain consciousness.
Pathology
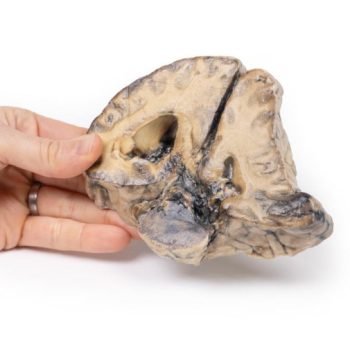
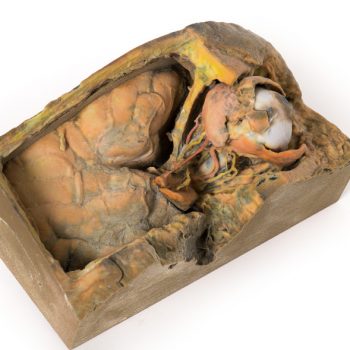
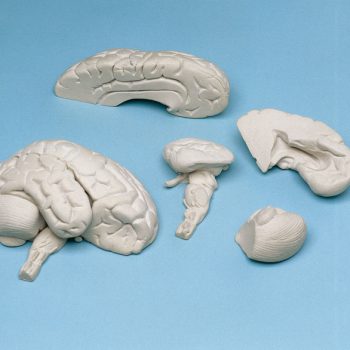
The specimen is a coronal section of a brain. It is evident that the brain has been compressed laterally and downwards by a right-sided expanding intracranial mass, probably a meningioma. The original mass is not present. The anterior face shows shift of midline structures with subfalcine herniation* of the cingulate gyrus. The posterior face (see photo) shows haemorrhage of varying ages within the temporal lobe and the pons, typical of supratentorial mass lesions. There is also ventricular asymmetry.
*In subfalcine (or cingulate) herniation, the most common type of brain herniation, the innermost part of the frontal lobe is pushed under part of the falx cerebri, between the two hemispheres of the brain.
Further information
Symptoms of a space occupying meningioma in the cranial cavity can be caused by the tumour mass pressing on the brain, which can lead to atrophy and displacement of brain parenchyma, leading to symptoms arising from interruptions to cranial nerve functions, blood flow and normal cerebral functions. General symptoms may include:
Muscle seizures: e.g. Myoclonic (single or multiple muscle twitches, jerks, and/or spasms) or Tonic-clonic (grand mal: loss of consciousness and body tone, followed by twitching and relaxing muscle contractions, loss of control of body functions, short period of no breathing and the person may turn a shade of blue, a person may be sleepy and experience a headache, confusion, weakness, numbness, and sore muscles)
Sensory changes – alterations in vision, smell, and/or hearing without losing consciousness.
Symptoms and signs may vary with the location of the tumor.