In Stock
Adenocarcinoma of the stomach
€1,290.00
Product information “Adenocarcinoma of the stomach”
Clinical History
An 82-year old female presents with an episode of melena (dark tarry faeces). She had a 6-month history of dyspepsia and nausea. Recently she had noted weight loss and early satiety. Soon after admission she had a large melena episode and died.
Pathology
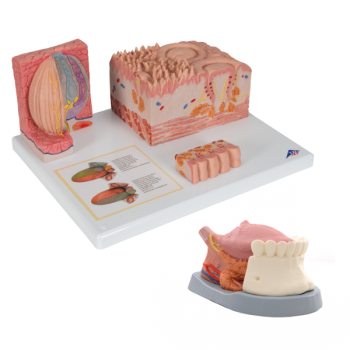
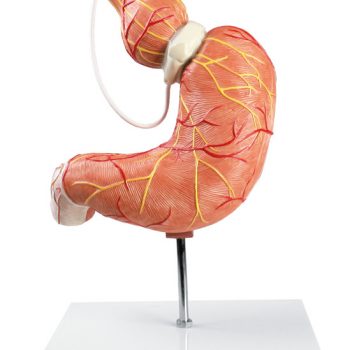
This is a post mortem specimen sliced to include a sagittal view of the oesophagus, stomach, proximal duodenum and pancreas. A large 7x5cm ulcer is evident on the lesser curve of the stomach. The ulcer is shallow and broad with raised rolled edges and necrotic debris at the base. There is loss of gastric rugae radiating along the mucous from the ulcer. Dissection of the ulcer reveals elevation of the edge by pale homogenous tumour tissue. There were two eroded arteries present within the ulcer crater with evidence of recent haemorrhage. The pancreas is adherent to the serosal aspect of the ulcer. Histology taken from the lesion (sites visible as regular 3cm defects) demonstrated an ulcerating, well-differentiated adenocarcinoma of the stomach with direct invasion into the pancreas.
Further Information
Gastric adenocarcinoma is the most common malignancy of the stomach. The incidence varies widely with geography: with a much higher incidence in Japan, Chile, Eastern Europe when compared to North America, Africa, South East Asia and Northern Europe. Risk factors include smoking, high salt diets, H. Pylori infection, Gastro Esophageal Reflux Disease (GERD), atrophic gastritis and intestinal metaplasia of the gastric mucosa.
There are two distinct classifications: intestinal and diffuse gastric adenocarcinoma. Intestinal adenocarcinoma resembles glandular tissue similar to colonic or oesophageal adenocarcinoma. Intestinal types tend to be bulky: growing as either an ulcerated or exophytic tumour. Intestinal type occur most frequently in endemic areas, has a male predominance and a mean age of 55 years at presentation. Intestinal type can occur from precursor lesions, such as dysplasia and/or adenomas with dysplasia. Diffuse type gastric cancers have an infiltrative growth pattern and are composed of ‘signet ring’ cells – i.e. cells that have large vacuoles full of mucin leading to displacement of the nucleus to the cell‘s periphery. The cells appear to have lost adhesion between each other, and can therefore be widely distributed within the stomach mucosa. A mass may not be appreciated in this diffuse type as a desmoplastic reaction can occur around the tumour cells, causing a thickened and rigid stomach wall with loss of rugae, creating a “leather bottle” appearance also know of linea plastica. Diffuse type has equal incidence across sexes and countries, and does not have precursor lesions. Germ line mutations in CDH1, which causing loss of function of E-cadherin leading to the loss of cell adhesion, can result in an increased risk of diffuse gastric cancer, which can be familial. Patients with Familial Adenomatous Polyposis (FAP) with germ line mutation in adenomatous polyposis coli (APC) gene have an increased risk in developing intestinal type gastric adenocarcinoma.
Early symptoms include dyspepsia, dysphagia and nausea. Later symptoms include weight loss, anorexia, early satiety, fatigue, anaemia and haemorrhage. Treatment depends on tumour stage with surgical resection for early tumours and chemotherapy for later stage cancers.