Product information “Multiple Renal Calculi”
Clinical History
A 68-year old male presented with fevers and rigors. Further questioning reveals a 6-month history of intermittent bilateral flank pain and haematuria. Biochemical investigations reveal significantly impaired renal function with a normal serum calcium. A CT abdomen showed bilateral hydronephrosis with multiple renal calculi as well as perinephric and subphrenic abscesses. He later died from progressive renal failure.
Pathology
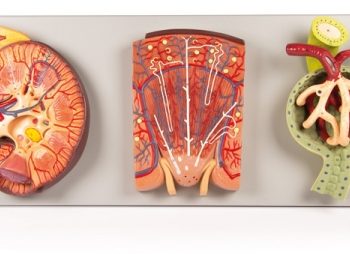
The specimen is patient’s kidney, which is grossly and partially bisected. There is gross dilatation of the pelvi-calyceal system visible. Significant atrophy of renal tissue can be seen, in some places being reduced to a mere rim. A large mottled brown-white calculus lies in the pelvis, and a smaller calculus occludes the ureter lumen. The ureter is dilated proximal to the impacted calculus. There are multiple calculi visible within the calyces of the specimen.
Further Information
Urolithiasis (renal calculi) is a very common disease affecting up to 1 in 10 individuals during their lifetime. Formation of the stones can occur anywhere along the urinary tract but most commonly occurs within the kidneys. Risk factors for stone formation include male gender; any condition that affects the composition of the urine, such as hypercalciuria or high urine oxalate; systemic metabolic disorders, such as cystinuria and gout; dietary factors, such as high oxalate and animal protein intake, low fluid intake; and environmental factors, such as high dry temperatures. 80% of renal calculi are unilateral.
Symptoms of urolithiasis include excruciating pain, haematuria, nausea, vomiting, fainting, dysuria and urgency. Symptoms depend on the size and the site of the calculus. Urolithiasis can be asymptomatic especially if the stones are formed and remain within the renal pelvis or bladder. Symptoms occur when the stones move into the ureter. Pain from calculi is usually colicky and typically severe in nature; occurring in paroxysms. The flank is the most common site for pain but pain can occur anywhere along the urinary tract and into the genitals. Pain resolves on passage of the stone. Haematuria can be gross or microscopic.
There are four main types of renal calculi:
Calcium stones are the most common, comprising 70% of all stones. They are made up of calcium oxalate or a mixture with calcium phosphate. Hypercalciuria, hypercalcemia and hyperoxaluria are common causes of these stones.
Struvite stones make up 5-10% of stones. They are comprised of magnesium ammonium phosphate. These are commonly formed as a result of proteus infections and lead to the formation of very large “staghorn” calculi.
Uric acid stones make up 5-10% of calculi. These occur in patients with hyperuricemia, such as gout and chronic leukaemias.
The remainder are made up of cysteine, which is due to impaired renal reabsorption of amino acids such as cystine.
Diagnosis can be made based on the medical history and examination. Radiological tools frequently used to assist diagnosis include non-contrast CT or ultrasound of the kidneys and bladder. Less commonly used imaging methods include abdominal X-ray, intravenous pyelogram and magnetic resonance imaging.
If left untreated renal damage and failure from progressive obstruction. Renal calculi also predispose patients to infection secondary to obstruction and trauma that they cause. Treatment in acute patients include supportive treatment to allow the passage of the stone. Medical treatment used includes analgesia, commonly NSAIDs and opiates, and agents to aid passage of the stone, such as alpha blockers, calcium channel blockers and antispasmodics. Surgical intervention may be required if there are severe complications due to calculi or if the stone is large and unable to be expelled with conservative treatment. Surgical interventions include lithotripsy (using lasers or electricity), laparoscopic stone removal or percutaneous stone removal. Open surgery is rarely required.